COMMON CONDITIONS OF THE WRIST
The information outlined below on common hand conditions is provided as a guide only and it is not intended to be comprehensive. Discussion with Ms Moon is important to answer any questions that you may have. For information about any additional hand and wrist conditions not featured within the site, please contact us for more information.
Some wrist fractures are stable. “Non-displaced” breaks, in which the bones do not move out of place initially, can be stable. Some “displaced” breaks (which need to be put back into the right place, called “reduction” or “setting”) also can be stable enough to treat in a cast or splint. Other fractures are unstable. In unstable fractures, even if the bones are put back into position and a cast is placed, the bone pieces tend to move or shift into a bad position before they solidly heal. This can make the wrist appear crooked.
Some fractures are more severe than others. Fractures that break apart the smooth joint surface or fractures that shatter into many pieces (comminuted fractures) may make the bone unstable. These severe types of fractures often require surgery to restore and hold their alignment. An open fracture occurs when a fragment of bone breaks and is forced out through the skin. This can cause an increased risk of infection in the bone.
CAUSES
A wrist fracture occurs from an injury such as falling down onto an outstretched hand. Severe trauma such as car accidents, motorcycle accidents or falls from a ladder cause more severe injuries. Weak bones (for example, in osteoporosis) tend to break more easily.
SIGNS AND SYMPTOMS
When the wrist is broken, there is pain and swelling. It can be hard to move or use the hand and wrist. Some people can still move or use the hand or wrist even if there is a broken bone. Swelling or a bone out of place can make the wrist appear deformed. There is often pain right around the break and with finger movement. Sometimes the fingers tingle or feel numb at the tips.
HOW IS THE DIAGNOSIS MADE?
Your hand surgeon will do a physical examination and obtain x-rays to see if there is a broken bone. Sometimes, tests such as a CT scan or MRI scan may be needed to get better detail of the fracture fragments and other injuries. Ligaments (the soft tissues that hold the bones together), tendons, muscles and nerves may also be injured when the wrist is broken. These injuries may need to be treated also.
WHAT IS THE TREATMENT?
Treatment depends on many factors, including:
• Type of fracture, whether it is displaced, unstable or open
• Your age, job, hobbies, activity level, and whether it is your “dominant” hand
• Your overall general health
• Presence of other injuries
A padded splint might be worn at first in order to align the bones and support the wrist to provide some relief from the initial pain. If the fracture is not too unstable, a cast may be used to hold a fracture that has been set. Other fractures may benefit from surgery to put the broken bones back together and hold them in correct place.
Fractures may be fixed with many devices. Pins, screws, plates, rods or external fixation can all be used. A small camera might be used to help visualize the joint from the inside. Sometimes the bone is so severely crushed that there is a gap in the bone once it has been realigned. In these cases, a bone graft may be added to help the healing process. Mr Mason will discuss the options that are best for your healing and recovery.
RECOVERY
During recovery, it is very important to keep your fingers moving to keep them from getting stiff. Your hand surgeon will have you start moving your wrist at the right time for your fracture. Hand therapy is often helpful to recover motion, strength and function.
Recovery time varies and depends on a lot of factors. It is not unusual for recovery to take months. Even then, some patients may have stiffness or aching. Severe wrist fractures can result in arthritis in the joint. Occasionally, additional treatment or surgery is needed.
What is it?
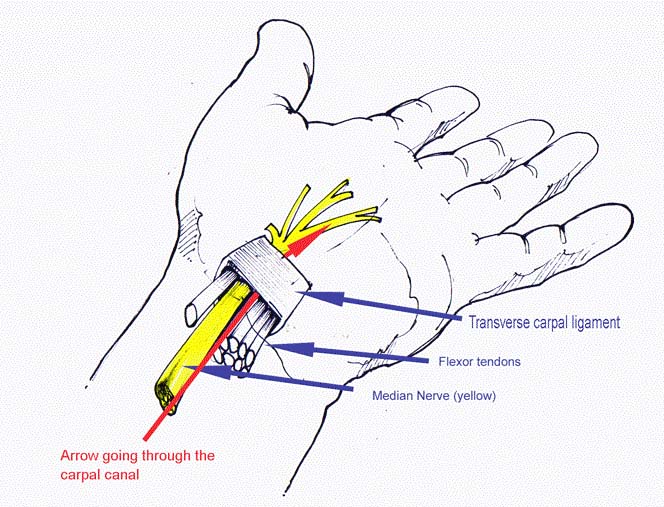
Carpal tunnel syndrome (CTS) is a condition where the median nerve is compressed where it passes through a short tunnel at the wrist. The tunnel contains the tendons that bend the fingers and thumb as well as the nerve (see diagram). CTS commonly affects women in middle age but can occur at any age in either sex. CTS can occur with pregnancy, diabetes, thyroid problems, rheumatoid arthritis and other less common conditions, but most sufferers have none of these. CTS may be associated with swelling in the tunnel which may be caused by inflammation of the tendons, a fracture of the wrist, wrist arthritis and other less common conditions. In most cases, the cause is not identifiable.
What are the symptoms?
The main symptom is altered feeling in the hand, affecting the thumb index, middle and ring fingers; it is unusual for the little finger to be involved. Many people describe the altered feeling as tingling. Tingling is often worse at night or first thing in the morning. It may be provoked by activities that involve gripping an object, for example a mobile telephone or newspaper, especially if the hand is elevated. In the early stages the symptoms of tingling intermittent and sensation will return to normal. If the condition worsens, the altered feeling may become continuous, with numbness in the fingers and thumb together with weakness and wasting of the muscles at the base of the thumb. Sufferers often described a feeling of clumsiness and drop objects easily. CTS may be associated with pain in the wrist and forearm.
In some cases, nerve conduction tests are needed to confirm the diagnosis. Blood tests and x-rays are sometimes required.
What is the treatment?
Non-surgical treatments include the use of splints, especially at night, and steroid injection into the carpal tunnel. CTS occurring in pregnancy often resolves after the baby is born.
Surgery is frequently required. The operation involves opening the roof of the tunnel to reduce the pressure on the nerve (see diagram: the roof of the carpal tunnel is called the transverse carpal ligament). The most common method involves an incision over the tunnel at the wrist, opening the roof under direct vision. In an alternative keyhole method (endoscopic release) the roof is opened with instruments inserted through one or two small incisions. The outcomes of the two techniques are similar and your surgeon can discuss the most appropriate method. The surgery may be performed under local anaesthesia, regional anaesthesia (injected at the shoulder to numb the entire arm) or general anaesthesia.
The outcome is usually a satisfactory resolution of the symptoms. Night pain and tingling usually disappear within a few days. In severe cases, improvement of constant numbness and muscle weakness may be slow or incomplete. It generally takes about three months to regain full strength and a fully comfortable scar, but the hand can be used for light activities from the day of surgery.
Arthritis involves inflammation of one or more of your joints. Pain and stiffness are common symptoms of arthritis, and when these occur in your wrist, simple daily activities can become more difficult. There are many types of arthritis, and most of these can affect the wrist. Although the severity of symptoms related to arthritis can vary, most arthritis-related diseases are chronic. This means that they are long-lasting—even permanent—and can eventually cause serious joint damage.
Your wrist is a complex joint—it is actually made up of multiple small joints. When healthy, the bones glide easily over each other during movement, protected by smooth cartilage that coats the joint surfaces. Arthritis damages this cartilage. As the disease progresses, there is a gradual loss of cartilage. Without a smooth joint surface, the bones rub against each other, leading to joint damage that cannot be repaired.
Although there is no cure for arthritis today, there are many treatment options available to help relieve your symptoms. Some options may also slow the progression of joint damage. With proper treatment, many people are able to manage their symptoms and stay active.
The wrist is a complex joint that connects the hand to the forearm. It is formed by the two bones of the forearm—the radius and the ulna—and eight small carpal bones. The carpal bones are arranged in two rows at the base of the hand. There are four bones in each row.
The joint surface of each bone is covered with articular cartilage—a slippery substance that protects and cushions the bones as you move your hand and wrist.
Although there are many types of arthritis, the three that most commonly affect the wrist are:
• Osteoarthritis
• Rheumatoid arthritis
• Posttraumatic arthritis
Osteoarthritis
Osteoarthritis can develop due to normal “wear-and-tear” in the wrist, particularly in people who have a family history of arthritis. It is a common problem for many people after they reach middle age, though it may occur in younger people, too. In osteoarthritis, the smooth, slippery articular cartilage that covers the ends of the bones gradually wears away over time. Because the cartilage surface has little to no blood supply, it has little ability to heal or regenerate when it becomes injured or worn down. As the cartilage wears away, it becomes frayed and rough, and the protective space between the bones decreases. This can result in bone rubbing on bone and lead to pain and stiffness in the joint.
Rheumatoid Arthritis
Rheumatoid arthritis is a chronic disease that can affect multiple joints throughout the body. The condition often starts in smaller joints, such as those found in the hand and wrist. It is symmetrical, meaning that it usually affects the same joint on both sides of the body. Rheumatoid arthritis is an autoimmune disease. This means that the body’s immune system attacks its own tissues. In rheumatoid arthritis, the defenses that normally protect the body from infection instead damage normal tissue (such as cartilage and ligaments) and can soften bone. Rheumatoid arthritis often affects the joint between the two bones of the forearm, the radius and ulna. The deformity in the ulna can cause wearing and possible rupture of the tendons that straighten your fingers. This can cause more deformity and loss of function in your hand. The exact cause of rheumatoid arthritis is not known—there are no clear genetic or environmental factors. Although it is not an inherited disease, researchers believe that some people have genes that could make them more likely to have rheumatoid disease.
Posttraumatic Arthritis
Posttraumatic arthritis can develop after an injury, such as a broken wrist bone or a torn ligament. This trauma can cause a direct injury to the cartilage or a delayed wearing of the cartilage due to a change in the way the bones move together—such as after a ligament tear. Posttraumatic arthritis can develop over many years from the initial injury. Despite proper treatment, an injured joint is more likely to become arthritic over time.
Not all patients with arthritis will experience symptoms. When they do occur, the severity varies greatly from patient to patient. For some patients, the symptoms are not constant—but may come and go depending on their level of activity and other factors.
Symptoms of arthritis may include:
• Pain
• Swelling
• Reduced range of motion or stiffness
• Weakness in the joint
There is no cure for arthritis, but there are a number of treatments that may help reduce the frequency of your symptoms and relieve the pain and loss of function it can cause.
Nonsurgical Treatment
In general, initial treatment for arthritis is nonsurgical in nature and designed to help minimize your symptoms. Nonsurgical treatment options may include:
• Activity modification. Limiting or stopping the activities that make your pain worse is the first step in relieving symptoms.
• Immobilization. Wearing a wrist splint for a short time will help support the joint and ease the stress placed on it by frequent use and activities.
• Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin, naproxen, and ibuprofen can help reduce both pain and swelling. Topical NSAIDs can be applied directly to the skin in the area of the joint.
• Exercise. Specific exercises will help improve range of motion and function in your wrist. Your doctor or a physical therapist can help develop an exercise program that meets your specific needs.
• Steroid injection. Cortisone is a powerful anti-inflammatory agent that can be injected into an arthritic joint. Although an injection of cortisone can provide relief and reduce inflammation, the effects may be temporary.
• Other therapies. This may include using “contrast soaks” of warm and cold water to help reduce swelling.
If your symptoms of rheumatoid arthritis are not adequately controlled by the above therapies, your doctor may prescribe additional medications. These medications—called disease-modifying anti-rheumatic drugs (DMARDs)—are designed to stop the immune system from attacking the joints.
Like all medications, DMARDs have both risks and benefits. Your use of DMARDs will be directed by a rheumatologist.
Surgical Treatment
If nonsurgical treatment does not relieve your pain and your quality of life has been significantly affected by arthritis, your doctor may recommend surgery. The goal of surgery is to relieve pain while preserving or improving hand function. Typically, this is done by minimizing or eliminating bone-on-bone contact. There are a number of procedures for arthritis of the wrist. Your doctor will talk with you about which procedure will work best in your case.
Proximal row carpectomy. In this procedure, your doctor removes three carpal bones in the row of bones that is closest to the forearm. The procedure is designed to reduce your pain while maintaining some wrist motion.
Fusion. If motion is the source of your pain, your doctor may recommend fusion. Fusion is essentially a “welding” process. The basic idea is to fuse together the bones so that they heal into a single, solid bone. The theory behind fusion is that, if the painful bones do not move, they should not hurt. During the procedure, your doctor removes the damaged cartilage and then uses pins, plates, or screws to hold the joint in a permanent position. Over time, the bones fuse or grow together— similar to the way the fractured ends of a bone heal together. In some cases, your doctor can perform a partial fusion in which just some of the carpal bones are fused together. This addresses the damaged joint surfaces, but leaves the healthy joints intact to preserve some wrist motion.
Total wrist replacement (arthroplasty). In total wrist replacement, your doctor removes the damaged cartilage and bone in your wrist and then positions new metal or plastic joint surfaces to restore the function of the joint. Replacing the wrist joint relieves the pain of arthritis while allowing more wrist movement than fusion.
De Quervain’s syndrome is a painful condition that affects tendons where they run through a tunnel on the thumb side of the wrist.

It appears without obvious cause in many cases. Mothers of small babies seem particularly prone to it, but whether this is due to hormonal changes after pregnancy or due to lifting the baby repeatedly is not known. There is little evidence that it is caused by work activities, but the pain can certainly be aggravated by hand use at work, at home, in the garden or at sport.
1. Pain on the thumb side of the wrist, as shown in the diagram. Pain is aggravated especially by lifting the thumb, as in the hitchhiker position or when using scissors.
2. Tenderness if you press on the site of pain.
3. Swelling of the site of pain – compare it with same spot on the opposite wrist.
4. Clicking or snapping of the tendons occurs occasionally.
De Quervain’s syndrome is not harmful, but it can be a really painful nuisance. Some mild cases recover over a few weeks without treatment.
Treatment options are:
1. Avoiding activities that cause pain, if possible
2. Using a wrist/thumb splint, which can often be obtained from a sports shop or a physiotherapist. It needs to immobilize the thumb as well as the wrist.
3. Steroid injection relieves the pain in about 70% of cases. The risks of injection are small, but it very occasionally causes some thinning or colour change in the skin at the site of injection.
4. Surgical decompression of the tendon tunnel. The anaesthetic may be local (injected under the skin at the site of operation), regional (injected in the armpit to numb the entire arm) or a general anaesthetic.
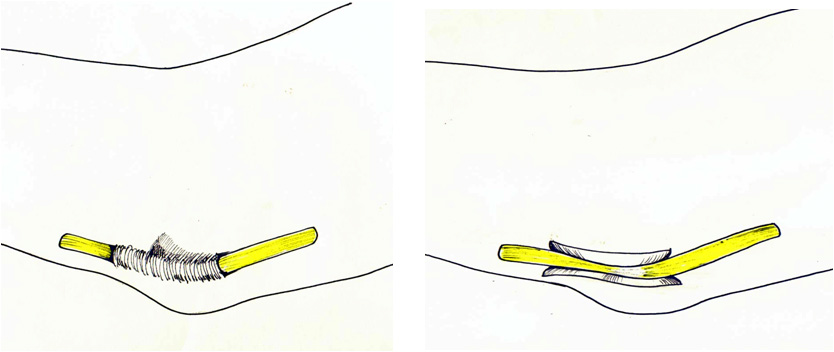
Through a transverse or longitudinal incision, and protecting the nerve branches just under the skin, the surgeon widens the tendon tunnel by slitting its roof. The tunnel roof forms again as the split heals, but it is wider and the tendons have sufficient room to move without pain.
Pain relief is usually rapid. The scar may be sore and unsightly for several weeks. Because the nerve branches were gently moved to see the tunnel, transient temporary numbness can occur on the back of the hand or thumb. Other risks are the risks of any surgery such as infection (less than one in 100 risk) or stiffness.
Download as an information leaflet (pdf)
What is it?
Cubital tunnel syndrome is compression or irritation of the ulnar nerve in a tunnel on the inside of the elbow (where your ‘funny bone’ is). The ulnar nerve provides sensation to the little finger and part of the ring finger, and power to the small muscles within the hand.
What are the causes?
Most cases arise without an obvious cause, but the tunnel can be narrowed by arthritis of the elbow joint or by an old injury.
What are the symptoms?
Numbness or tingling of the little and ring fingers are usually the earliest symptom. It is frequently intermittent, but may later become constant. Often the symptoms can be provoked by leaning on the elbow or holding the elbow in a bent position (e.g. on the telephone). Sleeping with the elbow habitually bent can also aggravate the symptoms.
In the later stages, the numbness is constant and the hand becomes weak. There may be visible loss of muscle bulk in severe cases, particularly noticeable on the back of the hand between the thumb and first finger, with loss of strength and dexterity.
Investigations may include x-rays of the elbow and nerve conduction studies.
What is the treatment?
Avoid or modify any provocative activity where appropriate. For example, wear a headset for using the telephone; avoid leaning on the inside of the elbows or wear protective pads. Excessive bending of the elbow at night can be minimised by a folded towel wrapped around the elbow, or by a splint provided by a therapist. These manoeuvres may be curative in early cases.
Surgery to decompress the nerve is required in severe cases, or in those that do not respond to the non-surgical treatments above. Surgery frequently improves the numbness, but its chief objective is to prevent the progressive muscle weakness and wasting that tends to occur in severe untreated cases. Several operations are used, including simple opening of the roof of the tunnel (decompression), moving the nerve into a new location at the front of the elbow (transposition) and widening the tunnel by removing some of its bony floor (medial epicondylectomy). Your surgeon can advise on the technique most appropriate to your problem.
What is the outcome?
The outcome depends upon the severity of the compression being treated. Numbness frequently improves, though the improvement may be slow. Surgery generally prevents worsening of the muscle weakness, but improvements in muscle strength are often slow and incomplete.
In the mild cases you can expect there to be full resolution of symptoms in most cases, the more severe the case the less predictable the long term outcome in regard to the nerve function fully recovering. Your surgeon and therapist should discuss the potential outcome with you.
Injuries caused playing tennis or skiing may not seem serious at first, but left untreated, can put athletes of all levels on the sidelines for months—and have a lasting effect on function. Sports-related hand injuries range from these apparently “minor” problems to those whose gravity is immediately evident, such as a fracture or dislocation to the wrist or finger joint. As noted, those associated with a specific activity or activities include:
• Skierʼs thumb (sometimes referred to as Game Keeperʼs Thumb), a highenergy injury in which the ligament at the base of the thumb is torn. This occurs when the patient falls forward and the thumb is bent backward.
• Tennis elbow, in which a tendon on the outside of the forearm fails and begins to tear away from the bone. While this injury originates near the elbow, pain may extend down the forearm.
• Golferʼs elbow, similar to tennis elbow, this injury affects the tendon on the inner side of the elbow.
• De Quervainʼs tendonitis, inflammation of the tendon that runs down the forearm, through the wrist, to the thumb. This injury is brought on by many activities including using a keyboard, golfing and fishing (particularly flyfishing).
• Wrist fractures, which can occur with many athletic activities; one of the most frequently seen injuries in beginning rollerbladers or snowboarders who tend to fall backward on their hands.
• Jamming a finger, or “basketball finger,” occurs during any athletic activity where the hand comes in contact with a ball. This injury ranges in severity from a sprain to a simple dislocation that may be corrected when the patient pulls on the finger to a more complex, serious dislocation or fracture of the joint.
• Tendonitis may also be seen in weight lifters with poor technique or in those who attempt to lift too much weight too soon. Similarly, beginning yoga practitioners may develop the problem by attempting postures that place too much stress on tendons that are not yet ready to accommodate it.
Regardless of the severity of the injury, prompt attention from an orthopedist can make an important difference in the patientʼs long-term recovery and ability to continue participating in sports. If the hand, wrist or finger is fractured, failure to get timely treatment will eventually result in arthritis and considerable pain.
Treatments
Fortunately, many of the injuries described can be treated with simple procedures that yield excellent long-term results. Jammed fingers that are dislocated can be relocated, that is, put back in proper alignment, often in the orthopaedic surgeonʼs office. If the finger is broken, the joint may need to be immobilized. A program of rehabilitation exercises helps patients prevent or reduce debilitating stiffness.
Skierʼs thumb can be treated with a simple procedure in which the ligament is reattached. This operation is done under regional anesthesia (the arm is numbed) and requires no hospitalization. Repairing this ligament is crucial since the thumb is responsible for about 50% of hand function, specifically for any movement that requires opposition, such as holding a cup or using a key. As with jammed fingers, timely treatment is essential. At three months following the injury, an orthopaedic surgeon may not be able to reattach the ligament and more complex surgery may be necessary.
Tendon injuries that result from persistent gripping of a racquet or golf club (or poor technique) or from numerous repetitions during weight lifting may be treated in a variety of ways. The affected joint may need to be immobilized. Therapy to decrease inflammation and swelling can include ultrasound treatments or iontophoresis. In the latter procedure cortisone cream is spread on the skin covering the affected area. A small electric charge is applied to get the cream to sink in and treat the muscles and tendons below. A cortisone injection or other antiinflammatory medication may also be needed. If these measures fail, surgery to open the tunnel or sheath that the tendon runs through, or in some cases remove the diseased tissue, may provide relief. Following surgery and recovery the patient receives instruction on how to alter their activities to avoid recurrence of the injury.
Treatment for fractures of the wrist or finger joints varies with the severity of the break. High energy, severe impact fractures, are often the most complex and may be comminuted (the bone is broken into many fragments.) These fractures may also be open, that is, the bone pierces the skin, and can carry a greater risk of infection. A range of treatments are available to patients. In the case of severe and otherwise untreatable fractures, including those not treated promptly, joint reconstruction or replacement may be viable options.
The information outlined below on common hand conditions is provided as a guide only and it is not intended to be comprehensive. Discussion with Ms Moon is important to answer any questions that you may have. For information about any additional hand and wrist conditions not featured within the site, please contact us for more information.






