COMMON CONDITIONS OF THE HAND
The information outlined below on common hand conditions is provided as a guide only and it is not intended to be comprehensive. Discussion with Ms Moon is important to answer any questions that you may have. For information about any additional hand and wrist conditions not featured within the site, please contact us for more information.
Download as an information leaflet (pdf)
What is it?
Ganglion cysts are the commonest type of swelling the hand. They contain a thick clear liquid called synovial fluid, which is the body’s lubricant in joints and in the tunnels through which some tendons run. Although ganglion cysts can arise from any joint or tendon tunnel, there are four common locations in the hand and wrist – in the middle of the back of the wrist, on the front of the wrist at the base of the thumb, at the base of a finger on the palmar side, and on the back of an end joint of a finger.
What is the cause?
A ganglion cyst arises when the synovial fluid leaks out of a joint or tendon tunnel and forms a swelling beneath the skin. The cause of the leak is generally unknown.
What are the symptoms?
A swelling becomes noticeable. It may or may not be painful.
How is the diagnosis made?
The diagnosis is usually straightforward as ganglion cysts tend to be smooth and round, change in size from time to time and occur at characteristic locations in the hand and wrist. If the diagnosis is uncertain, x-rays or scans may be helpful.
What is the treatment?
Ganglion cysts are harmless and can safely be left alone. Many disappear spontaneously and many others cause little trouble. For ganglion cysts in general, the possibilities for treatment:
1. Explanation, reassurance, wait to see if the cyst disappears spontaneously
2. Removal of the liquid contents of the cyst with a needle (aspiration) under local anaesthetic
3. Surgical removal of the cyst
For any individual cyst, the recommendations for treatment will depend on the location of the cyst and on the symptoms that it is causing.
Dorsal wrist ganglion cyst. Typically occurs in young adults and often disappears spontaneously. Aspiration can reduce the swelling but it often returns. The risk of recurrence after surgery is around 10%, and problems after surgery include persistent pain, loss of wrist movement and painful trapping of nerve branches in the scar.
Palmar wrist ganglion cyst. May occur in young adults, but also seen in association with wrist arthritis in older individuals. Aspiration may be useful, but care is needed as the cyst is often close to the artery at the wrist (where you can feel the pulse). The risk of recurrence after surgery is around 30%, and problems after surgery include persistent pain, loss of wrist movement and trapping of nerve branches in the scar. For these reasons, many surgeons advise against operation for these cysts.
Flexor tendon sheath ganglion cyst. Typically occurs in young adults, causing pain when gripping and feeling like a dried pea sitting on the tendon sheath at the base of the finger. Puncture of the cyst with a fine needle can disperse it – like puncturing a balloon – and fewer than half return. Persistent cysts can be removed surgically and the risk of recurrence is small.
Dorsal digital ganglion cyst. Usually in middle-aged or older people and associated with wearing out of the end joint of a finger. Pressure from the cyst may cause a furrow in the fingernail. Occasionally the cyst fluid leaks through the thin overlying skin from time to time. The risk of recurrence after surgery is around 10%, and problems after surgery include infection, stiffness and pain from the worn out joint.
What is it?
Trigger finger is a painful condition in which a finger or thumb clicks or locks as it is bent towards the palm.
What is the cause?
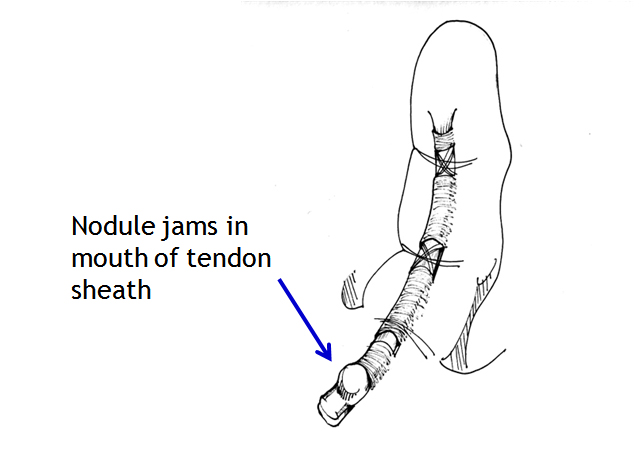
Thickening of the mouth of a tendon tunnel leads to roughness of the tendon surface, and the tendon then catches in the tunnel mouth. People with insulin-dependent diabetes are especially prone to triggering, but most trigger digits occur in people without diabetes. Triggering occasionally appears to start after an injury such as a knock on the hand. There is little evidence that it is caused by work activities, but the pain can certainly be aggravated by hand use at work, at home, in the garden or at sport. Triggering is sometimes due to tendon nodules in people known to have rheumatoid arthritis. It is not caused by osteoarthritis.
What are the symptoms?
1. Pain at the site of triggering in the palm (fingers) or on the palm surface of the thumb at the middle joint, usually in a person over the age of 40.
2. Tenderness if you press on the site of pain.
3. Clicking of the digit during movement, or locking in a bent position, often worse on waking in the morning. The digit may need to be straightened with pressure from the opposite hand.
4. Stiffness, especially in trigger thumb where movement at the end joint is reduced.
What is the treatment?
Trigger finger and trigger thumb are not harmful, but can be a really painful nuisance. Some mild cases recover over a few weeks without treatment. The options for treatment are:
1. Avoiding activities that cause pain, if possible
2. Using a small splint to hold the finger or thumb straight at night. A splint can be fitted by a hand therapist, but even a lollipop stick held on with tape can be used as a temporary splint. Holding the finger straight at night keeps the roughened segment of tendon in the tunnel and makes it smoother.
3. Steroid injection relieves the pain and triggering in about 70% of cases, but the success rate is lower in people with diabetes. The risks of injection are small, but it very occasionally causes some thinning or colour change in the skin at the site of injection. Improvement may occur within a few days of injection, but may take several weeks. A second injection is sometimes helpful, but surgery may be needed if triggering persists.
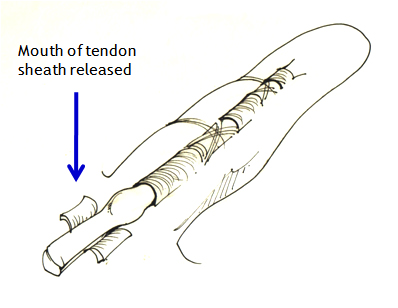
4. Percutaneous trigger finger release with a needle. Some surgeons prefer to release the tight mouth of the tunnel using a needle inserted under a local anaesthetic injection, but others feel that open surgery is more effective. The needle method is not suitable for all cases and all digits.
5. Surgical decompression of the tendon tunnel. The anaesthetic may be local (injected under the skin at the site of operation) regional (injected in the armpit to numb the entire arm) or a general anaesthetic. Through a small incision, and protecting nerves that lie near the tunnel, the surgeon widens the mouth of the tendon tunnel by slitting its roof. The wound will require a small dressing for 10-14 days, but light use of the hand is possible from the day of surgery and active use of the digit will aid the recovery of movement. Pain relief is usually rapid. Although the scar may be red and tender for several weeks, it is seldom troublesome in the longer term. Recurrence of triggering after surgery is uncommon.
Download as an information leaflet (pdf)
What is it?
Dupuytren’s contracture (also referred to as Dupuytren’s disease) is a common condition that usually arises in middle age or later and is more common in men than women. Firm nodules appear in the ligaments just beneath the skin of the palm of the hand, and in some cases they extend to form cords that can prevent the finger straightening completely. The nodules and cords may be associated with small pits in the skin. Nodules over the back of the finger knuckles (Garrod’s knuckle pads) and lumps on the soles of the feet are seen in some people with Dupuytren’s disease.
Why does it occur?
The cause is unknown, but it is more common in Northern Europe than elsewhere and it often runs in families. Dupuytren’s disease may be associated with diabetes, smoking and high alcohol consumption, but many affected people have none of these. It does not appear to be associated with manual work. It occasionally appears after injury to the hand or wrist, or after surgery to these areas.
What are the symptoms?
Dupuytren’s disease begins with nodules in the palm, often in line with the ring finger. The nodules are sometimes uncomfortable on pressure in the early stages, but the discomfort almost always improves over time. In about one affected person out of every three, the nodules extend to form cords that pull the finger towards the palm and prevent it straightening fully. Without treatment, one or more fingers may become fixed in a bent position. The web between thumb and index finger is sometimes narrowed. Contracture of fingers is usually slow, occurring over months and years rather than weeks.
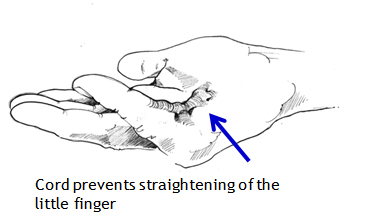
What is the treatment?
There is no cure. Surgery can usually make bent fingers straighter, though not always fully straight; it cannot eradicate the disease. Over the longer term, Dupuytren’s disease may reappear in operated digits or in previously uninvolved areas of the hand. But most patients who require surgery need only one operation during their lifetime. Published evidence does not support the use of radiotherapy. Injection of collagenase is helpful in some cases.
Surgery is not needed if fingers can be straightened fully. It is likely to be helpful when it has become impossible to put the hand flat on a table, and should be discussed with a surgeon at this stage. The surgeon can advise on the type of operation best suited to the individual, and on its timing. The procedure maybe carried out under local, regional (injection of local anaesthetic at the shoulder) or general anaesthetic.
Surgical options are:
1. Fasciotomy. The contracted cord of Dupuytren’s disease is simply cut in the palm, in the finger or in both, using a small knife or a needle (needle fasciotomy).
2. Segmental fasciectomy. Short segments of the cord are removed through one or more small incisions.
3. Regional fasciectomy. Through a single longer incision, the entire cord is removed. This is the most common operation.
4. Dermofasciectomy. The cord is removed together with the overlying skin and the skin is replaced with a graft taken usually from the upper arm or groin. This procedure is usually undertaken for recurrent disease, or for extensive disease in a younger individual.
After surgery, the hand may be fitted with a splint to be worn at night and a hand therapist may help with rehabilitation of the hand. The recovery is variable with regard to the degree of improvement achieved and the time to achieve the final position. The final outcome is dependent on many factors including the extent and behaviour of the disease itself and the type of surgery required.
Download as Information Leaflet
What is it?
The terminal joint of the finger is called the distal interphalangeal joint (DIPJ) (see diagram). Osteoarthritis often affects these joints, and can also affect the joint at the base of the thumb (Basal thumb arthritis). Osteoarthritis is loss of the smooth cartilage surface covering the ends of the bones in the joints. The cartilage becomes thin and rough, and the bone ends can rub together. Osteoarthritis can develop at any age, but usually appears after the age of 45. It may run in families.
What are the symptoms?
• Pain
• Swelling
• Deformity
• Stiffness
• Loss of function
Many peoples notice small bony bumps on the back of the joint. These are osteophytes, which are bony swellings associated with an osteoarthritic joint. In the hand they are called Heberden’s Nodes.
Many people with osteoarthritis of these joints have very little pain. Even though the joints may become lumpy and bent, the hands usually continue to work quite well.
What is the treatment?
Episodes of pain, redness and swelling frequently settle spontaneously over some weeks or months, and can be managed by avoiding painful activities (if possible), simple painkillers, anti-inflammatory gels or anti-inflammatory medication. Steroid injections are sometimes given.
Surgery can be used to fuse (stiffen permanently) a joint that is persistently painful, but the potential benefit needs to be balanced against the loss of movement. The joint is usually fused in a straight or slightly bent position.
There are various surgical techniques used to obtain fusion and your surgeon will explain the technique he or she plans to use for you. After the surgery you may need to wear a splint to support and protect the joint for several weeks.
Arthritis at the base of the thumb
Download as an information leaflet (pdf)
What is it?
The universal joint at the base of the thumb, between the metacarpal and trapezium bones, often becomes arthritic as people get older. It is osteoarthritis, which is loss of the smooth cartilage surface covering the ends of the bones in the joints. The cartilage becomes thin and rough, and the bone ends can rub together.
Osteoarthritis can develop at any age, but usually appears after the age of 45. It may run in families, and it sometimes follows a fracture involving the joint many years before.
Arthritis of the basal joint of the thumb is common in women and rather less common in men. X-rays show it is present in about 25% of women over the age of 55, but many people with arthritis of this joint have no significant pain.
What are the symptoms?
1. Pain at the base of the thumb, aggravated by thumb use.
2. Tenderness if you press on the base of the thumb.
3. Difficulty with tasks such as opening jars, turning a key in the lock etc.
4. Stiffness of the thumb and some loss of ability to open the thumb away from the hand.
5. In advanced cases, there is a bump at the base of the thumb and the middle thumb joint may hyperextend, giving a zigzag appearance.
What is the treatment?
The options for treatment include:
1. Avoiding activities that cause pain, if possible.
2. Analgesic and/or anti-inflammatory medication. A pharmacist or your family doctor can advise.
3. Using a splint to support the thumb and wrist. Rigid splints (metal or plastic) are effective but make thumb use difficult. A flexible neoprene rubber support is more practicable.
4. Steroid injection improves pain in many cases, though the effect may wear off over time. The risks of injection are small, but it very occasionally causes some thinning or colour change in the skin at the site of injection. Improvement may occur within a few days of injection, but often takes several weeks to be effective. The injection can be repeated if needed.
5. Surgery is a last resort, as the symptoms often stabilise over the long term and can be controlled by the non-surgical treatments above. There are various operations that can be performed to treat this condition. These are listed below:
a. Osteotomy, which means cutting and realigning the metacarpal bone next to the arthritic joint.
b. Removal of the trapezium which is removal of the bone at the bottom of the thumb, which forms one surface of the arthritic joint, sometimes combined with reconstruction of the ligaments.
c. Fusion of the joint, so that it no longer moves.
d. Joint replacement, as in a hip replacement.
e. Denervation, which means cutting small nerve branches that transmit pain from the arthritic joint. Removal of the trapezium is the most commonly performed operation. Ms Moon will advise you on the best options for your thumb.
A nerve injury can occur when the finger, hand, or wrist is cut, overstretched, crushed or burned. Symptoms include numbness and difficulty moving the affected area.
Treatment depends on the severity of the injury, and may include rest, immobilization, physical therapy, and in some cases, surgery.
Causes of hand & wrist nerve damage Injury to nerves in the hand or wrist is often caused by trauma, such as the area being cut, overstretched, crushed or burned, damaging the nerve or nerve ending.
Symptoms of hand & nerve damage
The nerves located in the hand and wrist affect motor and sensory functions. If a nerve in the hand or wrist is cut, severed, stretched, or otherwise damaged, it will not function properly (or at all).
Damage to motor nerves can cause weakness, twitching, and paralysis in the hand, wrist and arm. Sensory nerve damage symptoms include pain, numbness, tingling, increased sensitivity, burning, and problems positioning the hand correctly.
Similarly, when a nerve in the hand or wrist is pinched or compressed (such as in carpal tunnel syndrome), there can be pain and loss of feeling through the hand and fingers.
Treatment of hand & nerve damage
If the nerve is pinched or compressed, surgery may be able to release the nerve and restore functionality, depending on the severity of damage and how long the nerve was compressed.
If any of the tendons in your hand are damaged, surgery may be needed to repair them and help restore movement in the affected fingers or thumb.
What are tendons?
Tendons are tough cords of tissue that connect muscles to bones. When a group of muscles contract (tighten), the attached tendons will pull on certain bones, allowing you to make a wide range of movements.
There are two groups of tendons in the hand:
▪ extensor tendons – which run from the forearm, across the back of your hand to your fingers and thumb, allowing you to straighten your fingers and thumb
▪ flexor tendons – which run from your forearm, through your wrist and across the palm of your hand, allowing you to bend your fingers.
Surgery can often be carried out to repair damage to both these groups of tendons.
When hand tendon repair is needed Hand tendon repair is carried out when one or more tendons in your hand rupture or are cut, leading to loss of normal hand movements.
If your extensor tendons are damaged, you’ll be unable to straighten one or more fingers. If your flexor tendons are damaged, you’ll be unable to bend one or more fingers. Tendon damage can also cause pain and inflammation (swelling) in your hand.
In some cases, damage to the extensor tendons can be treated without the need for surgery, using a rigid support called a splint thatʼs worn around the hand.
Common causes of tendon injuries include:
• cuts – cuts across the back or palm of your hand can result in injury to your tendons
• sports injuries – extensor tendons can rupture when stubbing a finger, such as trying to catch a ball; flexor tendons can occasionally be pulled off the bone when grabbing an opponent’s jersey, such as in rugby; and the pulleys holding flexor tendons can rupture during activities that involve lots of strenuous gripping, such as rock climbing
• bites – animal and human bites can cause tendon damage, and a person may damage their hand tendon after punching another person in the teeth
• crushing injuries – jamming a finger in a door or crushing the hand in a car accident can divide or rupture a tendon
• rheumatoid arthritis – rheumatoid arthritis can cause tendons to become inflamed, which in severe cases can lead to tendons rupturing
Tendon repair surgery
Tendon repair may involve the surgeon making an incision in your wrist, hand or finger so they can locate the ends of the divided tendon and stitch them together. Extensor tendons are easier to reach, so repairing them is relatively straightforward. Depending on the type of injury, it may be possible to repair extensor tendons in an accident and emergency (A&E) department using a local anaesthetic to numb the affected area.
Repairing flexor tendons is more challenging because the flexor tendon system is more complex. Flexor tendon repair usually needs to be carried out under either general anaesthetic or regional anaesthetic (where the whole arm is numbed) in an operating theatre by an experienced plastic or orthopaedic surgeon who specialises in hand surgery.
Recovering from surgery
Both types of tendon surgery require a lengthy period of recovery (rehabilitation) because the repaired tendons will be weak until the ends heal together.
Depending on the location of the injury, it can take up to three months for the repaired tendon to regain its previous strength.
Rehabilitation involves protecting your tendons from overuse using a hand splint. You’ll usually need to wear a hand splint for several weeks after surgery.
You’ll also need to perform hand exercises regularly during your recovery to stop the repaired tendons sticking to nearby tissue, which can prevent you from being able to fully move your hand.
When you can return to work will depend on your job. Light activities can often be resumed after 6-8 weeks and heavy activities and sport after 10-12 weeks. Read more about recovering from hand tendon repair.
Post Operation
After an extensor tendon repair you should have a working finger or thumb, but you may not regain full movement. The outcome is often better when the injury is a clean cut to the tendon, rather than one that involves crushing or damage to the bones and joints.
A flexor tendon injury is generally more serious because they’re often put under more strain than extensor tendons. After a flexor tendon repair, it’s quite common for some fingers to not regain full movement. However, the tendon repair will still give a better result than not having surgery.
In some cases, complications develop after surgery, such as infection or the repaired tendon snapping or sticking to nearby tissue. In these circumstances, further treatment may be required.
The information outlined below on common hand conditions is provided as a guide only and it is not intended to be comprehensive. Discussion with Ms Moon is important to answer any questions that you may have. For information about any additional hand and wrist conditions not featured within the site, please contact us for more information.






